
We’re going to talk about sex, while traveling and not. This article gets into everything sexual health for people of all genders, and discusses sexually transmitted infection (STI) prevention and pregnancy prevention. Additionally, I break down sexual health while traveling locally and abroad, which is an important distinction because I believe that everything is more complicated when you are abroad versus in your own country with access to familiar resources.
I am not a medical professional. I am sharing knowledge that I have acquired through my own independent research. If you have a medical concern while at home or traveling, contact a doctor or other medical professional.
This article is not comprehensive, but I do try to give a brief overview of the many options available for STI prevention and pregnancy prevention, as well as tips for travelers regarding sexual health while traveling. Follow the links in blue for more information on every topic that I discuss below.
Finally, I view “sexual health” as having two components: that which is physical and that which is emotional/mental. This article will discuss the physical component. The emotional component (i.e. communication, comfort, consent) is equally important, and will continue to be discussed throughout this blog.
First of all… let’s define ‘sex’
‘Sex’ is shockingly ambiguous. The first step in the process is to forget the definition of sex that most of us have been taught from a young age: that sex is an act that occurs between a man and a woman, in which the man’s penis penetrates the woman’s vagina. This is one definition of sex, but it is not all-encompassing. Sex can occur between people with no vaginas, no penises, some XX parts and some XY parts, etc. Sex can involve hands, tongues, clitorises, anuses, vaginas, penises… basically, sex is broad and defined by the individual(s). It is important to draw attention to this because not everyone has penetrative, heterosexual, penis-in-vagina sex, but everyone is entitled to safe and healthy sex, information, and resources, regardless of the kind of sex that they are having.
In this article, I define sex as anything that occurs below the belt that involves bodily fluids.
STI prevention
You can minimize your risk of STI transmission and exposure by using barriers during sex. Common barriers include condoms (outside/male condoms and inside/female condoms), dental dams, and gloves and finger cots.

Male/outside condoms are a great option for STI prevention and pregnancy prevention
Outside/male condom: Used for sex involving a penis (or sex toy such as a dildo). It should cover the penis, from the head of the penis to the base of the shaft. Male/outside condoms should be applied to an erect penis. Properly used, male/outside condoms catch pre-ejaculatory fluids (“pre-cum”) and ejaculate (“cum”).
Inside/female condom: Used for sex involving a vagina. The inside condom can be inserted into the vagina up to eight hours before sex, and properly inserted, covers the vagina from the cervix to the vulva. It’s a good option for owners of a vagina who want to have agency over their condom use. Additionally, it may be a more comfortable option for penis owners during penis-in-vagina sex, as it does not grip the penis.
Dental dams: For safer sex involving mouths and tongues, i.e. oral sex. Dental dams can be used during cunnilingus (oral sex involving the vulva/vagina) and analingus (oral sex involving the anus, also known as “rimming”). The dental dam is a thin sheet of latex that gets draped over the vulva or anus. Just make sure that either the giver or receiver holds the dental dam in place during use, as it will not stay put by itself.
Gloves and finger cots: For safer manual sex, i.e. hand sex. Gloves cover the entire hand, and finger cots cover single fingers, like tiny condoms for your fingers. Gloves and finger cots are effective in avoiding the transmission of germs that could result from small cuts or infections on the hands.
Barrier methods are highly effective ways to minimize exposure to STIs. I encourage experimentation with your partner or partners about which options work best, and I also encourage an open dialogue about potential histories of STIs and STI testing. It is not necessarily comfortable to talk to your partner(s) about STIs, though an honest dialogue about the sexual histories of the participants and potential exposure to STIs is an important part of safe sex.
Additionally, every person is entitled to safe sex. Never, under any circumstances, is a person obligated to have sex with another person. If a partner objects to using a barrier and/or birth control during sex, you can refuse to have sex with this person. Sex should be safe, fun, and sexy for all participants; it should not be stressful or coercive.
For more information on safer sex using barrier methods, including how-to’s of male/outside condoms, female/inside condoms, dental dams, gloves, and finger cots, see this comprehensive article which goes into more detail about all of these topics.
Pregnancy prevention
There are so many options available for birth control. Birth control can be hormonal or non-hormonal, and can be used as-needed or be semi-permanent or permanent. The majority of birth control options are available for people who could could become pregnant; however, there are some options available for those who could impregnate their partner(s). Talk to your doctor or health care provider about which birth control option or options are best for you and your body. In the United States, Planned Parenthood is another great resource where one can go to get birth control, get tested for STIs, and speak with medical professionals, among other services.
Hormonal birth control
Hormonal birth control typically works by preventing ovulation (i.e., the release of an egg). Typical hormonal birth control methods include the oral contraceptive (the pill), the patch, the ring, the shot, the implant, and the IUS (intra-uterine system). These forms of birth control are highly effective at preventing pregnancy, but do not provide protection against STIs. Additional barrier methods are necessary for STI prevention.

Oral contraceptive pills
The pill: The oral contraceptive can contain the hormones estrogen and progestin, or just progestin. The pill prevents pregnancy by preventing ovulation and thickening the cervical mucus, which helps prevent the passage of sperm to the egg. The pill is taken daily, and is most effective when taken at the same time each day.
The patch: The patch is a form of birth control that prevents ovulation and thickens the cervical mucus. It is a small sticker that is applied to the body, either on the abdomen, buttocks, outer upper arm, or upper torso (excluding the breasts). During each menstrual cycle, three patches are worn. The patch is changed once a week (every 7 days) for three weeks, followed by one patch-free week. The patch is not affected by heat, humidity, or exercise.
The ring: The ring is a small, flexible ring that is inserted into the vagina. The ring releases hormones that prevent ovulation. Once inserted, the ring remains in place for three weeks (21 days), followed by one ring-free week. The wearer typically will not feel the ring once inserted, and it is uncommon that the ring interferes with sex.
The shot: The shot is an injection of progestin that prevents ovulation and thickens the cervical mucus. The user must receive the injection once every three months by a doctor or other health care provider.
The implant: The implant is a small tube that is inserted into the upper arm. The implant, once inserted, lasts for three years. It works by preventing ovulation and thickening the cervical mucus. The implant must be inserted and removed by a doctor or other health care provider.
The IUS: The IUS is a small, plastic, T-shaped device that is inserted into the uterus. The IUS releases progestogen, and prevents pregnancy by thickening the cervical mucus, thinning the uterine lining (making it less likely to accept an egg), and in some cases stopping ovulation. Depending on the brand, the IUS can remain in place for three to five years. It must be inserted or removed by a doctor or other health care provider.
Non-hormonal birth control

Inside/female condoms are another great option for pregnancy prevention and STI prevention
Non-hormonal birth control methods, also known as barrier methods, do not involve the alteration of hormones. Some forms of non-hormonal birth control also serve as barriers for STI prevention, such as male/outside and female/inside condoms. However, not all forms of non-hormonal birth control protect against STIs, so adequate barriers must also be used to prevent the transmission of STIs in conjunction with these forms of birth control. Typical non-hormonal birth control methods include male/outside condoms, female/inside condoms, spermicide, the diaphragm, the cervical cap, the vaginal sponge, the copper IUD (intra-uterine device), and female sterilization. For more information on male/outside condoms and female/inside condoms, see my STI Prevention section above; for everything else see below.
Spermicide: Spermicide is a cream, gel, film, foam, or suppository that prevents pregnancy by stopping the movement of sperm. It is inserted into the vagina and should cover the cervix. Perfectly used, approximately 15 out of 100 users will become pregnant (typically used, approximately 29 out of 100 users will become pregnant); thus, it is a better option than no birth control at all, but is more effectively used in combination with other forms of birth control, such as condoms, the diaphragm, the cervical cap, or the vaginal sponge. Spermicide is readily available and can be purchased in most pharmacies and supermarkets.
Diaphragm: The diaphragm is a flexible cup made from silicone. The diaphragm is designed for use with spermicide. The user puts spermicide inside of the cup and also around the rim of the diaphragm, and then it is folded and inserted into the vagina and should sit against the cervix. The diaphragm prevents pregnancy by blocking the cervix, and using spermicide to immobilize sperm. Perfectly used, approximately 6 out of 100 users will become pregnant (typically used, approximately 12 out of 100 users will become pregnant). The diaphragm is available in different sizes and must be fitted by a doctor or other health care provider. It is reusable and can last approximately two years.
Cervical cap: The cervical cap is a bowl-shaped device made from silicone. It contains a loop on one side to aid in removal. The cervical cap is designed for use with spermicide. The user puts spermicide inside of the cap and in the groove on the outside of the cap. The cap is then inserted into the vagina and should sit against the cervix, staying in place through suction. The cervical cap prevents pregnancy by blocking the cervix and using spermicide to immobilize sperm. Perfectly used, approximately 9 out of 100 users will become pregnant (typically used, approximately 20 out of 100 users will become pregnant). The cervical cap is less effective for users who have already given birth. The cervical cap is available in different sizes and requires a prescription. It is reusable and can last approximately two years.
Vaginal sponge: The vaginal sponge is a foam sponge that contains a spermicide. One side of the sponge contains a dimple that fits over the cervix; the other side contains a loop to aid in removal of the sponge. The sponge functions by blocking sperm from entering the cervix, and by immobilizing sperm through the continuous release of spermicide. Perfectly used, approximately 9 out of 100 users will become pregnant (typically used, approximately 12 out of 100 users will become pregnant). The vaginal sponge is less effective for users who have already given birth. The sponge is readily available and can be purchased at most pharmacies. The sponge is not reusable.
Copper IUD: The copper IUD is the non-hormonal counterpart to the hormonal IUS. It is a small, T-shaped device that is inserted into the uterus. The IUD is made from copper, which acts as a spermicide. The copper IUD can remain in place up to 12 years. It must be inserted by a doctor or other health care provider. It is one of the most effective forms of non-hormonal birth control, as less than 1 out of 100 users will become pregnant each year while using the IUD.
Female sterilization: Female sterilization (i.e., tube tying) is a permanent form of birth control. It is a surgical procedure in which the fallopian tubes (the tubes that connect the ovaries to the uterus) are cut or blocked. Female sterilization is a highly effective form of birth control, but should only be used by those who do not want to reproduce in the future.

“Plan B” emergency contraception available in the United States
The emergency contraception pill/”morning after” pill
The emergency contraceptive pill (also known as the “morning after pill” or “Plan B” in the United States) should not be used as a primary form of birth control. It is intended to be used in the case of “accidents”, i.e. if the condom breaks during penis-in-vagina sex, if the participants engage in unprotected sex, or in any situation in which exposure to semen could potentially result in a pregnancy. It is most effective within 72 hours (3 days) of the sexual activity, though according to Planned Parenthood, it can be used within 120 hours (5 days). However, it is most effective when taken as close to the sexual activity as possible. In the United States, Plan B can be purchased over the counter in most pharmacies, and you do not need a prescription to purchase it.
Birth control options for men
There are currently fewer birth control options for men than for women, though there are some options available. The simplest option for men is condom use, which is effective for pregnancy prevention and STI prevention. One permanent form of birth control for men is a vasectomy. A vasectomy is a surgical procedure in which the vas deferens (the duct that allows sperm to move from the testes to the urethra) are cut or blocked. Post-vasectomy, a man still ejaculates, but his ejaculate no longer contains sperm. Vasectomy is a highly effective form of birth control, but should only be used by those who do not want to reproduce in the future. Additionally, vasectomy does not protect against STIs, so it should be used in conjunction with other barrier methods for STI protection.
Sexual health for travelers
*This post may contain affiliate links. If you make a purchase through one of these links, I will earn a small commission at no extra cost to you!*
Sexual health for travelers begins before you even leave for your trip. Pre-departure, it’s a good idea to talk to your doctor about any potential health risks that you may have while away or abroad, as well as to make sure that you’re up to date on all of your necessary vaccines. Specifically regarding sexual health, you can talk to your doctor about vaccines for Hepatitis B and Human papillomavirus (HPV), which are two sexually transmitted diseases for which vaccines are available. Each vaccine requires a series of injections (three separate injections, typically one to two months apart), meaning that you need to allot approximately six months to have the vaccines fully administered.
Also, good pre- and post-departure protocol is to get yourself tested for potential STIs. Many STIs show no symptoms, so oftentimes the only way to know that you’ve been infected is to get tested. Getting tested is important and empowering. If you have an STI, you can get the necessary treatment, plus you can take adequate precautions with any sexual partners.
Talk to your doctor or health care provider about your birth control options. You want to make sure that you will have access to birth control while traveling. Depending on the length of your trip, this could mean bringing enough from home to last you the duration of your trip, or acquiring birth control while abroad. Certain forms of birth control, such as male/outside condoms, will be easy to find in any country, though other forms of birth control may be less accessible or need a doctor’s prescription. Talk to your doctor about your best options for keeping your body safe while traveling.
Additionally, keep in mind that some forms of birth control have specific storage requirements, i.e. they must be stored at room temperature, in a cool or dry environment, etc. This is another important thing to be mindful of when planning your birth control needs while traveling, as some tropical environments with wet and/or humid climates may be inadequate storage conditions for your birth control.
If you are trying a new form of birth control, it’s generally a good idea to give your body a few months to adjust to the birth control before traveling. This way, you will know if the form of birth control works for you, and if not you can continue exploring your options with your doctor or health care provider.
Here is a database with information on the brand, manufacturer, and available countries for most forms of hormonal birth control.
Additionally, here is a database containing the available brands and countries in which you can find emergency contraception (the “morning after” pill) and here is a list of emergency contraception availability by country.
Sexual health packing list
Travel bloggers love packing lists, so here is my recommended sexual health packing list:
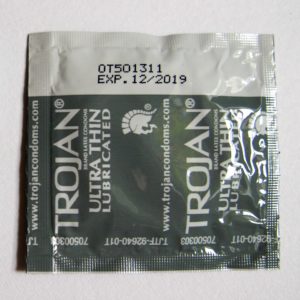
Condoms expire! Check the date before you go. 2.5 years left on this one…
Barriers for STI prevention (i.e. condoms, dental dams, etc.)
You know the drill. Choose your favorite or favorites (male/outside condom, female/inside condom, dental dams, gloves, finger cots, all of the above, etc.), check the expiration date (this is critical – these items do expire, and when expired they are much more brittle and likely to break), and pack a bunch.
- Birth control or other contraceptives
You will want to make sure that you have enough birth control to last you your trip, or a way of acquiring your form of birth control while abroad.
- Emergency contraception
Accidents during sex can be stressful enough. That, coupled with trying to find emergency contraception in a new environment (possibly a foreign country in which there are language barriers, etc.) might augment an already stressful situation. Emergency contraception is not a form of primary birth control, so I would consider this an optional item to carry. Carrying emergency contraception as a backup is essentially like investing 50 U.S. dollars upfront to not get pregnant. In the United States we can purchase Plan B, which lasts about two years before it expires (so make sure to check the date on your Plan B!). However, Plan B is expensive, so this is not necessarily a viable expense for everyone, especially if (hopefully) you don’t end up needing to use it.
- Pregnancy tests
Another optional travel item for those “just in case” scenarios, depending on finances and the length of one’s trip. If pregnancy tests are a viable expense, I recommend that longer-term travelers toss one or two into your bag, along with instructions in your native language.
- Condom carrying case

Rigid plastic condom carrying case
This is, quite possibly, the most ingenious invention ever. These compacts typically fit one or two male/outside condoms. An important component of condom use is that the condom does not get compromised in any way. For example, you should never use a condom that has been stored in a wallet, as the bending/motion/pressure on the wallet can cause the condom to deteriorate. This is where the condom carrying case comes in handy. They are made from rigid plastic, so no bending or breaking. You can safely store a condom, toss it into your backpack/purse/pocket, and have protection on the go. Costs about two dollars on Amazon, what a steal!
- Lube
Toss a big bottle into your checked luggage, or a travel size into your carry-on. Lube is a great way to make sex easier and more comfortable for any and all participants, as sometimes the body’s natural lubrication is not enough. Carrying lube is a way of having agency over your pleasure – use it with pride. However, make sure you pick up a bottle of water-based or silicone-based lubricant for use with condoms. Never use oil-based lube (such as baby oil, massage oil, or Vaseline) with condoms, as they break down the condom.
There you have it – my roundup of important information regarding STI prevention and pregnancy prevention, as well as some tips for local and international travelers regarding sexual health while traveling. Is there anything I can add to the list? If so, let me know in the comments below. Have fun and be safe!










